Good News for Ealing Hospital and some nice photos
|
||||||||||||||||||||||||||||||||||||||
 |
||||||||||||||||||||||||||||||||||||||
 |
||||||||||||||||||||||||||||||||||||||
 |
||||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||||
 |
||||||||||||||||||||||||||||||||||||||
 |
||||||||||||||||||||||||||||||||||||||
 |
||||||||||||||||||||||||||||||||||||||
|
The Downsizing of Ealing Hospital is a Past, Current and Future Threat
It is now apparent that the ‘hollowing-out’ of services at Ealing Hospital has been going on for over 10 years. This downsizing was brought into sharp focus when NHS North West London (NWL) published its ‘Shaping a Healthier Future’ (SaHF) plans in 2012. SaHF sounded the death knell for Ealing Hospital as a District General Hospital by mandating the closure of its Accident & Emergency (A&E) service in ‘at least three years’. It posited downgrading it from ‘Major Hospital’ status to ‘Local Hospital’ status.
Ever since the establishment of the Ealing Clinical Commissioning Group (ECCG) in 2013, this planning and purchasing body has shown little support for Ealing Hospital. In 2015 the ECCG closed down the hospital’s Maternity service and in 2016 it did away with Paediatrics.
In October 2014 Ealing Hospital Trust was dissolved and the hospital became a part of London North West University Healthcare Trust (LNWUHT). This Trust runs Northwick Park, Central Middlesex, St Mark’s and Ealing Hospitals. The Trust is headquartered at Northwick Park Hospital and during recent years the leadership of many healthcare services at Ealing Hospital has been transferred to Northwick Park.
On 26 March 2019, it was announced in Parliament that the SaHF plan was no longer supported by the Department of Health. The abandonment of this expensive failed plan seemed to suggest that Ealing Hospital’s A&E was saved and the downgrading/hollowing-out of Ealing Hospital would be terminated. However recent conversations with Ealing Hospital consultants along with information leaked from NHS NWL suggest otherwise.
When experienced professional staff leave Ealing Hospital they are often not replaced.
Incredibly there is no-one on-site who manages Ealing Hospital. Ealing Save Our NHS (ESON) asked LNWUHT bosses on 21 June 2019 for a list of services available at the hospital along with details of the level of service (e.g. consultants, surgery, specialised nursing). ESON asked for this as this information is not available on any NHS website. If patients have a right to choose where they are treated, they need to know where treatment is available! Three weeks on, the list has not been received by ESON.
At the June meeting with LNWUHT bosses, ESON asked for a copy of the post-SaHF plan for Ealing Hospital. No such plan exists but one is planned. September 2019 was the date promised for this plan. Apparently there are intentions to introduce some ’specialised services’ at Ealing Hospital. This same phrase and intention was voiced by Mark Easton, the NHS NWL boss at his meeting with ESON on 8 July 2019.
ESON made it clear to LNWUHT and NHS NWL bosses that nothing less than a development plan and formal re-launch of Ealing Hospital was needed.
If all the new flats being built and planned to be built in Ealing over the next 10 years ever get finished and occupied, the number of Ealing residents will rise from 345,000 now to over 400,000 by 2030. Not to have a fully functioning, sustainable major hospital in Ealing to service all these residents would be irresponsible and utterly shameful.
NHS NWL Proposes a Bewildering Array of Organisational Changes: Local Authorities are Expressing Significant Reservations
On 28 May 2019, NHS North West London (NWL) published a ‘Commissioning Reform’ paper on why replacing its eight local CCGs with one regional one was such a good idea. On 26 June 2019 an NHSE paper on Integrated Care System (ICS) design was published. On 10 July 2019 I was sent a set of NHS NWL slides the contents of which were an attempt to put more flesh on the bones of the May ‘case for change’ paper.
Feedback also exists from leaked comments from NHS NWL staff on 12Jjune 2019 and Local Authority Councillors speaking at the 21 June 2019 North West London Joint Health and Scrutiny Committee (JHOSC). At the JHOSC, Councillors expressed a wide range of concerns which included inadequate time to assimilate the changes for a 1 April 2020 start date, financial risks, budget organisation, how it will actually work in practice, cuts to services, no business case and staffing uncertainties. The most vociferous Councillors were those representing Hammersmith & Fulham, Hounslow, and Kensington & Chelsea. Shamefully no Ealing Councillors could be bothered to attend the meeting. Ealing Save Our NHS (ESON) met with NHS NWL supremo Mark Easton on 8 July 2019 and quizzed him on what and why was being proposed.
Why the Changes?
The overt reason for all the proposed changes is for NWL to comply with the January 2019 NHSE Long Term Plan (LTP). The LTP preaches that if care organisations work together then, as night follows day, we will enjoy improvements to our health provided by ’co-ordinated efficient services’.
However, surely with NHS Trusts and borough CCGs in deficit the changes must be driven by the desire to more successfully control costs? ‘Fixed (price) contracts’ was the term used by Mark Easton at the ESON meeting. The current ‘payment by results’ approach puts the incentives in the wrong place according to Mr Easton..
Back to the ‘working together’ approach – this is completely at odds with the ‘working apart’ approach of separating NHS purchasing from care service suppliers. This ‘market’ approach is one of the bedrocks of the 2012 Health & Social Care Act. One can only presume that after more than five years trying to get the separation/market approach to work it’s now deemed to be a failure.
What Are the Changes?
The first thing that strikes me is the high number of management bodies which will be created and will have to be maintained. Here’s a flavour:
+ Integrated Care System (ICS) Board
+ Clinical Commissioning Group (CCG) Governing Body
+ STP Partnership Board
+ ‘Place Teams’ – 8 of them
+ ‘Local Committees’ – 8 of them
+ Integrated Care Partnerships (ICPs) – 8 of them
+ Primary Care Networks (PCNs) management teams – at least 47 of them.
To unpack some of the new jargon, ‘Place’ means borough. ’Local Committees’ are borough subcommittees of the new CCG and have delegated commissioning authority. Each of the ‘Place Teams’ report to its borough Local Committee. It’s really unclear as to what the Place Teams will actually do
It is clear that ICPs will not exist as from day 1 (irrespective as to whether this is April 2020 or April 2021). Each borough ICP will be ’developed’ by the borough Local Committee. The future goal for the Local Committees is that they will be ‘absorbed’ by their ICP.
There are three choices as to how a borough Local Committee might operate. Basically this is all about how the NHS and Local Authorities might work together. Crudely the options are:
It seems that in NHS South West London option 2. is favoured, whilst in NHS South East London boroughs are likely to choose different options.
Some of the proposals are extremely difficult to understand. A flavour of this is as follows:
Under the slide heading ‘Primary Care at NWL and Place’ it states ‘This could mean in practice: Central NW London team supported by locally based primary care teams’.
One has to ask what teams are these? Is the ‘Central NW London team the new CCG – or something else? What are these ‘locally based primary care teams’? Are they Place Teams, Local Committees PCN teams or ad hoc teams?
The reader is then presented with two options:
‘A single primary care commissioning team, for NWL, delivered by primary care leads (from CCGs), the NHSE commissioning/ finance teams, Enhanced Services team etc., to agree service plans, outcomes and financial envelope with local integrated care partnership (ICP) teams’.
For a start under the new reform regime there won’t be ‘CCGs’ – only just one at regional NWL level. What is ‘Enhanced Services team’? Is this pharmaceutical (introduced in 2013) and/or Directed Enhanced Services e.g. a PCN contract – introduced on 1 July 2019?
The other approach option is:
‘CCG-based teams to commission integrated care at a place-level as the PCNs mature alongside the core general practice commissioning requirements, overseen by local PCC and /or ’Committee-in-Common’. This model enables local ICPs to evolve alongside local general practice and PCN development over the 5 years of the PCN contract’.
‘Committee-in Common’ is a confusing and surreal concept. It’s where two or more organisations meet in the same place at the same time. However the two organisations remain distinct and (if the committee is decision making) take their own decisions. It’s hardly an example of progressive ‘working together’.
I have been researching/writing about NHS plans, processes and legislation in some detail now for over six years. I am also reasonably well educated but I have to say that I do not have the faintest idea what either of these options actually means.
There are plenty of references to the NHS NWL Sustainability & Transformation Plan (STP), parts of which are obsolete (e.g. the closure of Ealing Hospital A&E). Mark Easton did accept that following the demise of SaHF and the requirements of the January 2019 NHSE Long Term Plan (LTP), NHS NWL would adopt a single new plan – the NHS NWL LTP – some time later this year.
There is plenty of ‘Shaping a Healthier Future’ type aspirational verbiage including the old chestnut of ’more than 30% of patients in Acute hospitals shouldn’t be there’. However there’s nothing in the current reform proposals that reflects the chronic shortage of doctors, nurses, consultants and care support workers. No reference is made to the enormous building maintenance backlog and the desperate need for capital so that many of the NHS NWL hospitals don’t fall apart. Local Authority Social Care hardly gets a mention.
How Do NHS Staff Feel About the LTP and NWL’s ‘Commissioning Reform’ Proposals?
On 24 June 2019 the Doctors’ Union – the British Medical Association (BMA) – voted to oppose the NHS LTP describing it as ‘a plan for a market-driven healthcare system’. The BMA also opposed the shift of care from hospitals to the community. The BMA, formed in 1832, has over 100,000 members.
On 12 June 2019, some 500 NHS NWL staff were treated to an away day at which the NWL LTP/ reform proposals were presented to them. A whistle-blower released on-line comments and reactions to the slide show and the questions and answers sessions. These 100+ comments and responses from the staff revealed an unhappy workforce worried about their jobs, redundancy, incomplete information on how the reform might actually work, stress, bullying, overwork, need for a single IT system, unrealistic QIPP plans, vacancy and recruitment freezes, and money wasted on contractors, interims, agency staff, project managers and on the away-day itself! There is also an intriguing comment about Hillingdon is not being involved in the restructuring.
Public Consultation and Local Accountability
There are plenty of references to ‘engagement’ with key stakeholders in the NWL material, but there is no commitment whatsoever to formal public consultation on the reform plan. Twice I have asked Mark Easton face-to-face about whether ICPs will meet in public. Neither time did I get a straight answer. It’s probably important to discover whether the ICS, ICPs, Place Teams, Local Committees and PCNs will meet in public. If it’s just the NWL CCG which meets in public, then local activist organisations – like ESON in Ealing – will find it very hard to hold the NHS to account locally. This is especially true for Ealing as currently its only hospital does not hold performance review/information meetings in public at the hospital.
What Might Happen Next?
‘Key stakeholders’ are currently being ‘engaged’ and ’final engagement events to design proposals’ are planned for August 2019. Comments are welcomed up to 24 August 2019. Delegated budgets, management costs, outline structures and staffing intentions are being assembled and will be added to the reform plans. The eight statutory NHS NWL CCGs will be asked to approve the reform plans by October 2019. If all the CCGs give the green light then ‘change management’ and ’implementation’ will follow with the NWL preferred target start date for ’merge CCGs’ in April 2020.
There’s plenty that could de-rail this chain of events. Candidates for disruption include one NWL CCG saying ‘no’, a new Prime Minister and Cabinet, a no deal Brexit, a new Brexit referendum and a new Labour Government.
No ICP contracts have been signed and although 14 ICSs appear to ‘exist’ on paper surely none of them are single CCG post-LTP entities and will only be legitimised and formally activated when legislation to amend the 2012 Health & Social Care Act comes into force. The much trumpeted pioneer ICSs at Greater Manchester and at Dudley have been stalled for months. Dudley doesn’t even feature in the NHSE 14 ‘plastic’ ICSs! Parliament has been in a state of chaos for months and this chaos is likely to continue for many more months. My bet is that changes to the 2012 Act are unlikely to take place any time soon.
m
|
|||||||||||||||||||||||||||||||||||
 |
|||||||||||||||||||||||||||||||||||
 |
|||||||||||||||||||||||||||||||||||
|
Yet Another Major NHS Re-organisation: Will It Lead To Better Care Outcomes And/Or Significantly Reduced Management Costs?
On 28 May 2019 NHS North West London’s (NWL’s) Collaboration of Clinical Commissioning Groups (CCGs) published a 24 page draft document called ‘Commissioning Reform in North West London: the case for change’. This non-statutory body is proposing changes not just about who purchases care services but who manages care service delivery. Before these changes can be proposed to NHS England, the eight statutory NHS NWL CCGs will have to agree to them.
The context of this ‘case for change’ is the contents of the January 2019 NHS England’s Long Term Plan (LTP). On page 29 of the LTP it states ‘…..a single CCG for each ICS area.’ There is no business case in the LTP to support this massive organisational requirement. I can’t find a simple compelling reason in the LTP for the more than likely dismemberment of some 148 CCGs nationally. Is the case for change that after six years local CCGs have proved to be a failed initiative? In NWL it’s certainly the case that three of the eight CCGs are bankrupt. In the year 2018/19 the combined excess over expenditure of the eight NWL CCGs was £147,185,000.
We have to put this proposed reformation in the context of a chronic shortage of medical staff especially of doctors, nurses and mental health staff. There’s also the tragedy of social care being starved of money and much domiciliary care being of poor quality. We must also accept that seven years of the Acute reconfiguration transformation (‘Shaping a Healthier Future’) have ‘hollowed-out’ some of our District General Hospitals, especially Central Middlesex, Hammersmith and Ealing Hospitals.
One other truth that NHS NWL bosses still find hard to accept is that Type 1 (the most seriously ill) attendances at NWL hospital A&E units were lower in 2018/19 than they were in 2011/12. And this is over a period when the NWL population rose by 10%.
I have to point out that of the nine signatories/authors of this document, four of them were also signatories/authors of the ill-fated, £235 million 2012 NHS NWL ‘Shaping a Healthier Future’ project which was abandoned by the Department of Health on 26 March 2019.
Once, and if, all this is agreed it could become a reality on 1 April 2020 or 1 April 2021. It seems that three of the five London ‘footprints’ have decided on a 1 April 2020 start. It seems highly likely that by 1 April 2021 the current 192 CCGs across England will have been whittled down to just 44.
The Eight ‘Local’ CCGs in NWL are to be Terminated
The eight statutory NHS NWL CCGs, created in 2013 to meet the requirements of the 2012 Health & Social Care Act, are to be disbanded. However well or badly these purchasing bodies have performed over the last six years, they at least were ‘led’ by local GPs with local knowledge of the ‘town’ in which they operated.
All the CCG senior staff will no doubt lose their jobs. Losing eight CCG Chairs, CEO/COOs, HR, PR and Financial Directors will save a few £million in annual salaries alone. Or will they all be re-hired to run the eight new Integrated Care Partnerships (ICPs)? One wonders what will happen about the ’underlying’ deficit of the eight CCGs which in March 2019 stood at £99.6 million. Will it be ‘inherited’ by the new regional CCG?
And what about the 832 permanent staff employed by the CCGs ? The document speculates that ‘….there are likely to be few redundancies’. This seems hard to fathom on the face of it, as one can’t envision all or most of the staff at the eight CCGs joining the new CCG. What seems likely though is that CCG staff will move over to become ICP staff.
The annual ‘employee/workforce benefits’ in 2018/19 for all eight CCGs totalled £80.113 million. At the 19 June 2019 Ealing CCG meeting NHS NWL Accountable Officer Mark Easton quoted the total CCG cost to be £45 million. Where that figure comes from is a mystery to me. He seemed to suggest that this management cost was understandable given that NHS NWL turnover was £3 billion. He said management costs last year were reduced by 10% and that this year they would be reduced by another 10%. (There is a commitment in the document for costs to be reduced by 20%).
New NWL Integrated Care System (ICS)
The NWL ICS will, apparently be the whole care commissioning and service delivery shooting match. It appears that the 30 strong NHS NWL Health and Care System (HCS) will morph into the new NWL ICS board. Of course the NWL HCS is the re-named NWL Sustainability & Transformation Plan/Partnership (STP). In 2016, Ealing Council and Hammersmith & Fulham Council refused to sign the STP. Hence neither Council is formally represented on the NWL HCS. Will the two Councils finally relent and formally join the NWL ICS? It seems that Hammersmith & Fulham Council has concerns about the changes and has commissioned an independent review of what’s being proposed.
The graphic on page 5 states the NWL ICS will ’manage performance and £’. If this is the case, what is the new NWL CCG’s role with regard to managing performance and money? Surely the CCG is responsible for assigning priorities and purchasing all the care services for 2.2 million people? Is the CCG going to be just the purchasing department of the ICS?
A New Regional CCG (NWL CCG) Will Purchase All Care Services for 2.2 Million People in NWL
Presumably this will (like its eight predecessors) be a membership organisation. If so it will have 379 members (all the GP practices). One wonders whether the PCNs will also be members?
This ‘reform’ appears to be seriously at odds with the spirit and possibly the literal requirement of the 2012 Act for local commissioning. Will care commissioning be improved if it’s ’remote’ from the point of need, and service provisioning? Who will run this body, who will staff this body and how will the new NWL CCG bosses be chosen?
Eight New Local Integrated Care Partnerships (ICPs) Will Manage All Care Service Delivery in NWL
Presumably these ICPs will report to the new NWL CCG. No doubt local NHS Trusts, Primary Care Networks (PCNs), Local Authorities, charities, private care and voluntary organisations will variously report to these ICPs. Just how happy will these service providers be having an intermediate organisation sitting between them and the new commissioning body? Just how will this work in practice?
Apparently these ICPs will be both delegated commissioners and service provider managers. In Ealing, for example, WLNT delivers Secondary mental health and out of hospital services, LNWUHT delivers Ealing Hospital services, the seven PCNs will manage the 76 GP practices and Ealing Council supplies social services. So what will the Ealing ICP actually do? Where will the commissioning ‘split’ be made between the new CCG and each of the eight ICPs?
Is the plan to transfer many of the current local commissioning (CCG) staff to these new local service delivery (ICP) organisations? Will all these new jobs be advertised and multiple candidates interviewed? Or will staff just be transferred from one purchasing body role to a different purchasing and service delivery management organisation in the same town?
A view expressed by a senior NHS NWL executive is that these changes are aimed at ‘putting care closer to the patient’. However when this person was asked about the role of ICPs no answer at all was forthcoming.
‘…we will be moving away from the distinction between provider and commissioner’
This policy appearing on page 21 of the document really took my breath away. If this becomes reality then the 2012 Act will have been trashed. Believe me, I want the market system of separating purchaser and provider to be discontinued, but this must be done formally by Act of Parliament.
However at the 19 June 2019 Ealing CCG meeting, NHS NWL head honcho Mark Easton gave strong hints that the new CCG would delegate some of the commissioning to the new ICPs. It also came across that what the re-organisation was perhaps aiming at was more local control of service delivery (with the eight ICPs).
Healthwatch Inappropriately Described As a ‘Partner’ to ’Engage With’
The actual definition of the word ‘partner’ in a business context involves shared risk, shared profits and shared losses. Very often in the NHS this partner sharing is often non-existent. With regard to Healthwatch even the NHS’s careless use of the word is out of order. Healthwatch exists to hold NHS bodies to account. Healthwatch does not exist for NHS bodies to ‘engage’ with it. Currently some CCGs pay their local Healthwatch to deliver services. This is completely inappropriate and outrageous. Let’s hope the new NWL CCG does not pay money to its statutory ‘critical friend’.
Primary Care ‘Developments’
Many people feel Primary Care is regressing not developing. In 2012 they could get a GP appointment in days – now it takes weeks. I view with great cynicism the possibility of the aspirations being championed in this document becoming a reality anytime soon.
Page 22:
‘…GPs supported by Primary Care Networks (PCNs) in partnership with local community services, mental health and social care.’
It’s not clear what ‘local community services‘ are for a start. In Ealing, mental health and social care services are very thin on the ground and are stretched to breaking point. There’s hardly anything there to ‘partner’ with.
‘….mental health…can be managed by the local GP, practice nursing staff, community pharmacists and PCN effectively’
Anecdotally few GPs have any in-depth knowledge of mental health diagnosis and treatment. We are so far removed from GPs managing mental health that it’s really quite offensive to even propose this.
Page 23:
‘Our practices will work together in our PCNs. Our PCNs will operate through multi-discipline working delivering population health management, and support our ICPs to deliver the required health and care to our local population. These networks will be the bedrock of local/borough-level arrangements’.
I have read this through many times. Organising multi-discipline teams of staff from different organisations is difficult and expensive. Attempts to implement this team approach in NWL hospitals have largely been abandoned. Shouldn’t the ICP be supporting its PCNs? Exactly what will the relationship be between the PCNs and their ICP?
At best this motherhood and apple pie aspiration is meaningless. At worst it’s just unclear how these ICS/CCG/ICP/PCN processes and relationships are going to work at all, never mind improve outcomes and cut costs.
I’m sure there will be many more times in the coming months when we’ll hear about the virtues of ‘integration’, ‘co-commissioning’, ‘co-production’, ‘partnering’, ‘team approach’ and ‘multi-discipline’. Whether things will become any clearer is debatable. No doubt the real intentions behind creating these new structures and moving staff around into new jobs will become apparent over time.
NHS Admits That One in Eight Children Have a Mental Health Disorder: The Children’s Society Research On Waiting for Mental Health Treatment Makes Grim Reading
A quarter of 11 – 16 year-olds with a mental health disorder have self-harmed or attempted suicide. The figure rises to 46% amongst teenage girls. The Children’s Society charity has also released data obtained through Freedom Of Information research. It has discovered that in 2017, 106,000 10 – 17 year-olds were diagnosed with a mental health problem – but not treated. The target time for treatment for children is four weeks. However the research revealed that the average waiting time was 12 weeks. Even worse in some areas, children experiencing issues such as anxiety, depression and self-harm were waiting much longer – up to 364 days – for referral to first treatment. The charity is not impressed by the Government’s plans for mental health support in schools. It says as little as 20% of schools would benefit from the planned pilots.
Early Intervention Services For Children’s Mental Health Have Been Cut in More Than One Third of England.
An investigation by the Children’s Commissioner has revealed that prevention schemes like school counsellors, drop-in centres and online counselling designed to intervene before mental health issues become severely debilitating, even life-threatening, are now inaccessible.
Sadly children’s mental health problems and treatments have not improved much in recent years. In 2004 the Government revealed that one in 10 children in England had a diagnosable mental health problem. By 2015 the number of children being treated for mental health problems had doubled compared to 2010. In January 2018 NHS England/NHS Digital reported that the number of children self-harming was up annually by 385% over 10 years. At the same time the Department of Education reported that one in three 14/15 year old girls were suffering from a mental health illness. This was extracted from data in a 10 year study of 30,000 girls.
The Government in October 2018 announced an annual uplift of £2 billion for mental health services. In 2018/19 the annual mental health spend was £12.2 billion – around 10% of the total annual healthcare spend in England. However, the increase is dependent on the Government achieving a Brexit deal.
However one must pose the question – if this extra cash is forthcoming will it all definitely be spent on mental health services? A new regional integrated Care System (ICS) for each of the 44 English NHS ‘footprints’ is to be created. Local CCGs are to be disbanded and new regional CCGs created. At a local level new Integrated Care Partnerships (ICPs) will be set up. This effectively creates the opportunity for three levels of NHS executives to ‘slice and dice’ money available for physical health, mental health and social care.
|
|||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||
 |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
 |
||||||||||||||||||||||||||||||
|
‘GP at Hand’ with 51,596 Patients Threatens to Destabilise NHS Services in London
GP at Hand, Babylon Health’s virtual GP practice, has in just 18 months signed up and retained 51,596 patients. However, the ‘GPonline’ web site tells us that between November 2017 and March 2019 one in four of its patients had subsequently left the GP at Hand practice. 85% of those who signed up were aged between 20 and 39, and just over half of them were aged between 20 and 29.
GP at Hand is a Smartphone based app which facilitates online GP consultations at short notice. When you sign up to the virtual service, your registration at your place-based GP practice is cancelled. GP at Hand’s clinics include two in Fulham, a BUPA Health Clinic in Kings Cross, Lyca Health in Canary Wharf (part of the Lyca mobile phone operation), and one, the South Westminster Centre for Health, in Vincent Square. The latter appears to be run by diagnostic imaging specialists InHealth whose Cardiology Unit appears to have a link with Chelsea and Westminster Hospital.
In what the ‘Pulse’ web site describes as ‘destabilising’, it seems GP at Hand is in the process of registering its own NHS Primary Care Network (PCN). The aim of PCNs is collaborative working between GP practices, community, mental health, social care, pharmacy, hospital and voluntary services. Seven such PCNs have just been set up in Ealing. Each PCN can service up to 50,000 registered patients. GP leaders have expressed concerns that this ‘digital-first’ service will break the rule that PCN’s must exist within local boundaries. They predict that if virtual GP practices can become PCNs then it would destabilise all current NHS services in London.
We still await the results of the evaluation of GP at Hand carried out by Ipsos Mori which was first promised in March 2019. Publication of the results has been delayed three times now. NHS England and Hammersmith & Fulham (H&F) CCG commissioned this research which cost £250,000. The results were scheduled to be announced at the H&F CCG meeting on 21 May 2019. The presentation was cancelled at one hour’s notice, the CCG citing concerns about ‘factual accuracy’. Ipsos Mori, a 40 year old global leader in market research operating in 89 countries, is unlikely to be guilty of ‘factual inaccuracy’. However, ‘GPonline’ quotes Ipsos Mori researchers saying that ‘necessary datasets’ have not been made available to them.
Here we have a non-NHS provided service ‘approved’ by NHSE and personally endorsed by the Secretary of State for Health and Social Care. Maybe there are other virtual GP surgery offerings – maybe not. Apparently competitors include ‘Livi’ and ‘Push Doctor’. Have they (and possibly others) been ‘approved’ by NHSE? Perhaps GP at Hand should be nationalised and all GP surgeries mandated to offer it to all their patients. This would create a level playing field. Currently we have a tilted playing field which does not favour place-based GP surgeries in Hammersmith & London and elsewhere who are losing patients to GP at Hand.
GP at Hand appears to have a virtual monopoly in the virtual GP Surgery market. Although it is not illegal in England to set up a monopoly it is illegal to maintain one. Does Matt Hancock MP realise that by his publicly endorsing GP at Hand he is enabling the maintenance of a monopoly?
H&F CCG are facing an annual deficit of £37 million, 21.6 million of which stems from funding the growing patient lists of Fulham-based Dr Jefferies’ GP at Hand practice.
On 2 June 2019 ’The Sunday Times’ revealed worrying data about Babylon Health retrieved from the professional networking service ’LinkedIn’. Although high staff turnover rates are not unusual at tech star-ups, the fact the 37% of Babylon staff stay for 6 months or less is a real concern.
And Now We Have Virtual A&E…..
On 24 May 2019 ‘The Guardian’ exclusively revealed that sick patients in Birmingham will soon be able to seek emergency treatment by using their Smartphone instead of going immediately to a hospital A&E unit. They will engage in a two minute online triage to check their symptoms. This is yet another example of ‘demand management’ at work (see story below). The plan is to persuade 30% of those currently attending a place-based A&E to use a virtual A&E instead.
Not surprisingly Matt Hancock’s favourite ‘digital-first’ technology company Babylon Health is involved. A modified version of GP at Hand will be adopted by the University Hospitals Birmingham NHS Trust. The technology will be used to reduce face-to-face consultations in the areas of outpatients, chronic disease management (diabetes and heart problems) and in triage for Non-Elective hospital admissions.
NHS Says Charging for Nurse Training Will Result in 68,500 Unfilled Nursing Vacancies by 2013/24
The ‘Interim NHS Staff Plan’ has just been leaked and it makes worrying reading. It alleges that following the Government’s decision to abolish training bursaries for nurses, applications for nurse and midwifery training fell by 31% from 2016 to 2018. Clearly these dire predictions about staff shortages must have an impact on implementing the NHS Long Term Plan
The NHS Chief Executive Argues Against Policies He Has Championed
Simon Stevens has recently spoken in public about preventing the ‘hollowing out’ of District General Hospitals (DGHs). This is from the man who had allowed NHS North West London to hollow out Central Middlesex, Hammersmith and Ealing DGHs. The former two had their A&Es closed down in September 2014, and Ealing Hospital has in recent years been stripped of Maternity, Paediatrics, children’s A&E and Urology.
Delivering a lecture at the Royal Society of Medicine (RCM) in May 2019, Mr Stevens suggested that the NHS rethinks the DGH model to counter the risk of the health service deserting the ‘at risk communities’ many of them serve. This is all a bit rich when one considers that the hollowed-out Ealing Hospital is located in Southall, one of the most deprived areas in England.
Is what he is saying that he got it wrong in the past and he’ll put it right in the years to come? Well there’s nothing on in the ten year ‘NHS long Term Plan’ (LTP) published in January 2019 about reversing the hollowing out of DGHs.
So….how do we resolve these conflicting NHSE statements in the LTP and in the RCM lecture?
Is the Incidence of ‘Demand Management’ Initiatives a Potent Symbol of Neo-Liberal Dogma Permeating the NHS?
The concept of ‘demand management’ has a lot to do with ‘market’ situations when supply is dwindling – by design, by incompetence or by accident. Demand management initiatives somehow attempt to divert, bamboozle or even ‘educate’ the demander, resulting in their demands not being met or supply being delayed. If chocolate bars become in short supply demand management could raise prices or it could point out that too much chocolate is bad for you and offer the demander fruit (in greater supply) instead.
In the NHS since at least 2010, reducing the number of District General Hospitals (DGHs) and the number of hospital beds has been a design mandate. Hospitals are expensive places to run and NHS bosses started downgrading DGHs and reducing bed numbers as a way to cut costs. In NHS North West London (NWL) in 2012 bosses accepted the wisdom of management consultants McKinsey & Co that 40% of patients in Acute beds should not be there. Reducing bed numbers by 40% was the plan, but this plan was finally abandoned in March 2019. However in the 28 May 2019 NHS NWL commissioning reform paper, we are told that 30% of patients in Acute beds should not be there.
Whether by design, incompetence or accident, the number of doctors and nurses at work in the NHS is inadequate. In April 2019 NHS Improvement announced there were 100,521 NHS staff vacancies in England.
Various demand management techniques have been tried to reduce the number of people attending and being admitted to hospital. These include:
+ efforts to treat patients at home or in doctors’ surgeries (instead of in hospital)
+ attempts to make people lead healthier lives
+ initiatives to detect and treat potentially serious illnesses in their early stages which reduces the need for patients to enter intensive care in hospital
+ telephone voice and Smartphone online triage and treatment – hoping this will deter patients from turning up at GP surgeries, hospital Urgent Care Centres and hospital A&E departments.
+ ‘referral facilitation’ – slowing down, changing, or rejecting GP patient referrals to see hospital consultants
Some of these techniques have proved successful and some have failed.
If you want to see your usual GP it’s not unusual these days to have to wait three weeks for the privilege. Two requests in recent years for over £70 million to expand some GP surgeries in North West London have fallen on deaf ears at NHS England and the Department of Health.
Government smoking bans have been successful in reducing self-harm through nicotine/tar ingestion. However campaigns aimed at reducing self-harm from many other forms of substance abuse have had little success.
Initiatives with the elderly in detecting early stage bowel cancer, encouraging them to have flu jabs and self-checking their blood pressure at home have no doubt enjoyed some success. However there have been few publicised successful initiatives in detecting and treating early onset mental illnesses in children of all ages.
The jury is still out as to whether virtual GP surgeries, e.g. GP at Hand, are safe and effective and whether they might prove to be a universal panacea in Primary, Community and Secondary Care demand management.
In Ealing a referral facilitation service has been operating for a few years. A second GP reviews your GP’s referral for you to see a consultant. Well, it’s just been decided to discontinue this service in Ealing as allegedly it was proving to be a waste of money.
In the current NHS Long Perm Plan (LTP) the new Primary Care Networks (PCNs) will be financially rewarded if there are reductions in Acute hospital admissions amongst their 30,000 to 50,000 registered patient populations.
Also in the LTP, PCNs are expected to form multi-discipline teams to visit and treat patients at home in attempts to reduce the number of patients attending and being admitted to DGHs. This multi-discipline team approach has been tried throughout NHS North West London in recent years. Anecdotally I hear that it has been largely abandoned as it proved difficult to organise.
Reducing ‘bed blocking’ has gained much press attention in recent years. But has much been achieved in reducing it? At Ealing Hospital bed blocking, often by mentally ill and elderly patients, has effectively reduced the available beds even more. Because the number of specialist mental health beds have been reduced it’s often very difficult to discharge seriously ill mental patients. Government cuts to Local Authority funding have often resulted in much reduced care home capacity and home care services, sometimes making it impossible for recovering elderly patients to be safely discharged from hospital.
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
PLEASE SIGN OUR PETITION HERE
|
NHS Integrated Care Providers (ICPs) – Do They Exist? When Will They Exist?
The public consultation on the ICP contract ended on 26 October 2018. By now ICP contracts should have been signed in Dudley and in Greater Manchester. However I can find no news announcements or web site updates announcing such events. NHS England’s (NHSE’s) web site states that ‘….the ICP contract…in its updated form…available…from Spring 2019’. So – can we expect this within the next few weeks? Probably not as the NHS consistently misses its self-imposed deadlines.
For the confused, NHSE seems to use the terms ICP and ICS as and when it chooses. The two acronyms apparently are interchangeable.
Of course what happens every few years in the NHS these days is that its bosses throw all the balls up in the air. This latest ball throwing happened in January 2019, with publication of the NHS Long Term Plan (LTP). The ten year LTP replaces the October 2014 NHS Five Year View. The LTP states that ‘ICSs are central to the delivery of the LTP’; ‘By April 2021 ICSs will cover the whole country’; ‘A single CCG for each ICS area’. In February 2019 NHSE set out its desire to bring in new Government legislation to make it easy for new NHS Trusts to be set up to become ICS/ICPs. On the ground in NHS North West London (NWL), a new care commissioner will have to be created – the NWL Clinical Commissioning Group – to which the new contracted NWL ICS/ICP will be accountable.
The LTP also points the way towards a transformation in Primary Care. A separate NHSE/BMA January 2019 paper outlines these imminent changes. I review this paper later in this newsletter.
Another aspect of the LTP with regard to CCGs is the appointment of the Accountable Officer. The LTP states that NHSE will ‘designate the Council’s Chief Executive or Director of Adult Services as the CCG Accountable Officer’. This would eliminate the current NHS NWL Collaboration of CCGs Accountable Officer Mark Easton as a candidate in the new NWL CCG and open up the choice of eight Local Authority Chief Executives and eight Local Authority Adult Services Directors as candidates.
The LTP goes into ‘blue sky’ mode by predicting ‘….future proposals for social care and health integration in the forthcoming (Government) Green Paper on adult social care’. This paper was first promised for publication in summer, then ’before the end of 2018’ and now goodness knows when. However as social care is such a mess one might question the usefulness of the five Governmental Social Care Green Papers published since 1999.
NHS NWL’s 2012 ‘Shaping a Healthier Future’ (SaHF) Cancelled and NHS NWL’s 2016 Sustainability & Transformation Plan (STP) to be Abandoned – One Wonders What the Life Expectancy Will Be of the Yet To be Born NHS NWL ‘Long Term Plan’ (LTP)
At the latest meeting of the NHS North West London (NWL) Collaboration of the Eight Clinical Commissioning Groups (CCGs) on 2 May 2019 there was much line drawing under the SaHF and the STP. The new kid on the block in terms of a plan will be NHS NWL’s regional version of the NHS England (NHSE) LTP published in January 2019. However NHS NWL has been slow to even respond to the new national ten year LTP never mind engage with local stakeholders in formulating an NWL LTP. Healthwatch – allegedly the patients’ consumer watchdog – is being employed to collect feedback on the LTP. See www.healthwatch.co.uk/what-would-you-do.
Ground-breaking commitments were made at this meeting by NHS NWL bosses to active engagement with Ealing Save Our NHS (ESON) and Save Our Hospitals – Hammersmith (SOH) in formulating this regional LTP. However, the well publicised (but possibly not well advanced), plan by NHS NWL to select a 4,000 person standing panel to review ongoing care transformations is as yet not in place.
I’m very supportive of the KONP critique of the national LTP (see below) and I’m concerned that the NWL regional version will just ’parrot’ the national version. However of much more tangible significance was the announcement that in 2019/20 the NWL financial plan involves cutting its £3.6 billion annual costs by £100 million. If achieved, this will mean lots of ‘demand management’ initiatives to ration care.
Yet more turbulence is expected in NHS NWL this year as it wrestles with eliminating eight local CCGs and creating a new regional CCG. Sadly some quite well paid executives will fall off their lucrative CCG gravy trains. However only confusion appears to be the target of the body which might deliver the new CCG’s purchased services. The emerging regional Integrated Care Partnership/Integrated Care System (ICP/ICS) will attempt to bring together a host of care service suppliers – NHS Trusts, Local Authorities, private care companies, charities, voluntary groups. Attempts to achieve this ‘seamless’ co-operation have been hampered in the past by Local Authority opposition of SaHF and the STP, especially in Ealing and Hammersmith & Fulham.
As for apportioning blame for the £235 million spent on the now cancelled 2012 SaHF and the no doubt tens of £millions spent on the about to be abandoned 2016 STP, Accountable Officer Mark Easton said at the meeting that ’no-one was to blame’. I didn’t know whether to laugh or cry at that point in the meeting.
To discover that money is being spent on refurbishing NHS NWL headquarters offices in Marylebone Road, London seems massively inappropriate. This was the location of SaHF staff and not only that, there is a repair bill backlog of £729 million for just four of the NHS NWL Major Hospitals.
The Transformation of GP Services – The Story So Far
It’s now over six years since I began researching and reporting on changes to NHS healthcare services nationally, regionally and locally. During this period the term ‘transformation’ has gained popularity with NHS bosses to label these changes. How has transformation impacted GP services since 2013?
Waiting Times
No-one will dispute that waiting times to see a GP have got considerably longer since 2013. Lots of reasons have been suggested for this. These include an increase in demand from an ageing population having multiple medical conditions/ illnesses. On the supply side GP numbers have declined since 2015, and we have only marginally more GPs this year than last year.
Overworked GPs
A recent survey by ‘Pulse’ magazine/web site revealed that GPs are seeing up to 60 patients a day – double the number they consider safe.
A Post Code Lottery for Performance?
One way of profiling GP surgery performance is to research the number of annual Non-Elective (NEL) admissions to hospital per 1,000 Weighted Patients in each surgery, town or across the region. These NEL admissions are mostly Emergency admissions. Local researcher Tony Brewer has revealed that using the NHS’s own data there are more than double the number in Ealing (80.8) compared with Westminster (32.81). There are even wide variations across Ealing itself – with patients at surgeries in Acton (68.80) registering much lower NELs than across the rest of Ealing (from 73.15 –88.95)
GP Referrals to Consultants
In 2013 if your GP in Ealing referred you to a consultant, an appointment was made and you’d go to see the consultant. These days life is just not that simple. Every GP referral is intercepted by the Referral Facilitation Service (RFS). The RFS, run by a private contractor, will employ a GP to ‘second guess’ your GP. This intercepting GP could cancel the referral, change the referral or allow the referral. One can only presume that the RFS is all about reducing the number of GP referrals and cutting costs. In management consultancy jargon this approach to rationing a service supply is referred to as ‘demand management’.
Use of Technology
For those with mobile phones the texting service by GP surgeries has clearly helped with reminding patients about their appointments and expediting follow-ups to test results. Relatively inexpensive blood pressure monitors have been purchased by patients and this cuts down visits to surgeries just to have your blood pressure checked. However some technology use is proving disruptive and some question its efficacy. Babylon Technology’s ‘GP at Hand’ is the main culprit here.
GP at Hand
Introduced in London in 2017 this Smartphone-based virtual GP surgery has now more than 48,000 patients. Online consultations are available 24/7 at short notice. The original service was operated out of Dr Jefferies’ surgery in Fulham. numerous ‘place-based’ GP surgeries have lost patients and NHS funds to Dr Jefferies.
Concerns about the online service are varied. Pregnant women and mentally ill patients are seemingly not welcome as patients. Some question the effectiveness and safety of the service and others see it as a threat to place-based GP surgeries. NHS England and Hammersmith & Fulham (H&F) CCG invested £250,000 with Ipsos Mori in 2018 to carry out a full scale, year-long review of GP at Hand. The research report was promised by March 2019. No sign of it yet but NHS England has already agreed to an expansion of the service to Birmingham. H&F CCG has gone into considerable debt, largely as a result of having to pay-out £26.2million to Dr Jefferies for his new patients (many presumably out of Borough) in 2018 – 2020.
Clinical Commissioning Groups CCGs)
In recent years Ealing’s 76 GP surgeries have been commissioned by Ealing CCG. Given that the 2012 Health & Social Care Act created CCGs as GP-led it’s been astonishing that conflict of interest seemingly plays no part in Ealing GP-led CCG purchasing of Ealing GP services!
Ealing GP Federation (EGF)
This private company, in which all 76 Ealing GP surgeries are shareholders, did not exist in 2013. Founded in October 2014 this non-statutory body ‘…allows for greater collaboration between practices’. Its web site provides few clues as to why the federation actually exists.
The Transformation of GP Services – The Future Does Not Look Promising
In January 2019, NHSE and the BMA published ‘Investment and evolution: a Five-year framework for GP contract reform to implement the NHS Long Term Plan’. Some of the GPs who found time to read and digest this 108 page/50,000+ word document have expressed their dismay about its content. If the framework is implemented, they say, it will lead to a deteriorating and rationed GP service and move us closer to adopting a US style privatised healthcare system. However, some GPs welcome any attempts to enable GP co-operation and believe change is desperately needed.
An extra £4.5 billion is apparently to be invested in community-based care (however that is defined) by 2023/24. At the heart of the new ‘framework’ is yet another new GP contract – The Primary Care Network Contract (PCNC). There is a guaranteed additional payment of £1:76 per patient if /when GPs sign their PCNC. Each GP must sign this contract by 30 June 2019 (it was originally 15 May 2019 – but this is normal NHSE re-scheduling….). Activation was scheduled for July 2019 – no doubt this will get re-scheduled also. This contract promises GPs more money – but at what ‘cost’?
GP practice patient lists must be handed over to the GP’s Primary Care Network (PCN). Each PCN will comprise 30,000 to 50,000 patients. The PCNs report to the regional Integrated Care System (ICS) and the lists will be available to the ICS. Each PCN will have an Accountable Clinical Director. How the PCN in Ealing will relate to the Ealing GP Federation is somewhat unclear.
GPs will have to take on new tasks. These include structured medication reviews, Care Home visits, anticipatory care, personalised care, supporting early cancer diagnosis, cardio-vascular disease prevention and diagnosis, and tackling inequalities. GP appraisals and revalidations will take up valuable GP time. GP performance and activities will be monitored to ensure that GPs are adhering to ‘corporate policy’. Detailed electronic patient records will have to be kept and electronic dashboards will monitor everything and will form the basis for evaluating what GPs get paid.
GPs will be financially incentivised to reduce the number of patients admitted to Acute hospitals. They will also be part of multi-disciplinary teams which will visit sick patients at home in order to prevent Acute hospital admissions. GPs will not lead these teams and the teams will follow protocols and pathways. There are obvious conflicts of interest issues here for GPs if they feel their patient should be hospitalised and the system ‘says no’. There will be sharing of cost savings but the savings will not go to the GPs they will go to the PCN.
More staff will be hired, trained and paid for, but these will mostly not be GPs. 20,000 additional staff are promised by 2023/24. They will include pharmacists, paramedics, physiotherapists, mental health therapists, associate physicians, social care prescribing link workers, and specialist receptionists. In this way Primary Care in England will become de-professionalised. There is a recommitment to the historic NHSE promise to recruit 5,000 more GPs but an acceptance that this amounted to only a ’marginal’ increase in 2017/18.
All patients will, apparently, have digital access to their full medical records from 2020. It’s interesting to point out here that £11 billion was wasted in failing to implement online medical records access from 2002 to 2013 – and now it’s being offered next year!
Virtual GP practices are to be encouraged and expanded. By 2021 every patient will be able to join a virtual GP practice and have online consultations with a GP. In view of the chaos and disruption cause by 48,000 GP at Hand patients in West London, who knows what chaos and disruption to place-based GP practices will occur when we have say five million virtual GP practice patients throughout England? With the massive elimination of face-to-face patient consultation with the same doctor, continuity of care comes to an end. Online consultations are unlikely to ever take place with the same GP.
Just how much does the general public, the press, NHS staff and GPs themselves know about these transformation plans and their implications? If GPs don’t sign up to the new contract, how will they be ‘punished’ one wonders?
KONP Advocates Scrapping Section 75 in the 2012 Health & Social Care Act; Discontinuing Any Form of Competitive Tendering; and an End to the Market System in the NHS
In its submission to NHS England (NHSE) – responding to the NHS Long Term Plan and draft primary legislation public consultation – Keep Our NHS Public (KONP) wants an end to Section 75. Section 75 enforces compulsory tendering. In fact KONP wants an end to any form of competitive tendering and the dropping of the market system which separates purchasers from service suppliers. KONP points out that whilst it agrees with the proposal to remove the Competition and Markets Authorities role, it disagrees with NHSE seeking powers to force through mergers. Mergers have led to centralisation, cost cutting and remote decision making.
KONP is also opposed to the ‘Payment by Results’ system. It sees this as breaking up block contracts and service level agreements – leading to NHS services being outsourced to private providers. Integrated Care Provision in the form of new NHS trusts ‘…to deliver integrated care’ is seen by KONP as more of the disintegrated services that we have now. Finally, KONP wants the repeal of the 2012 Act and advancement of the NHS Reinstatement Bill.
KONP was founded in 2005. See http://keepournhspublic.com for more.
| Judging by the continuous stream of messages that we have received over the last few weeks, there is no doubt about the delight felt by people across the Borough that Ealing Hospital is to remain as a proper acute hospital. A very popular theme in many messages was that ‘we stood together as a united community’. A bit of People Power goes a long way – something that the Government and NHS bosses never understood. They thought we would all give up eventually, but they were so wrong! |
| After 7 years of hard work by so many people it’s fantastic to be able to celebrate, so Ealing Save Our NHS is having a celebration. We are therefore inviting those of you who helped in any way to achieve this great success for our community, to join us. There will also be hospital staff and local politicians, all raising a glass together! |
| Get in touch for more information! |
| Our planned Street Stall this Saturday in Ealing Broadway, 11.00 – 1.00pmnear M&S has a very different message then usual! |
| Instead of ‘Save Ealing Hospital, Dump SaHF ‘, our latest leaflet (here) now reads: |
| Of course, NHS bosses have refused to admit they have retreated, or for that matter offered any apology for the scandalous waste of money (at least £72 Million). Nor have they apologised for the closure of maternity & acute children’s services or the demoralisation of staff at Ealing Hospital. We certainly won’t be letting them off the hook, and intend to fight on to stop the threat of future cuts and restore our lost vital services. |
| If you can help give out leaflets on Saturday that would be great. It will be lovely to give people some good news at last. |
| Ealing Save Our NHS and our sister campaign, Save Our Hospitals (Hammersmith & Charing X) are featured on the front page of the national ‘Health Campaigns Together’ newspaper. We are both part of a family of campaigns up and down the country and together we have kept up the pressure on health bosses and the Government against cuts to hospitals and privatisation. |
| You can read the story and more here |
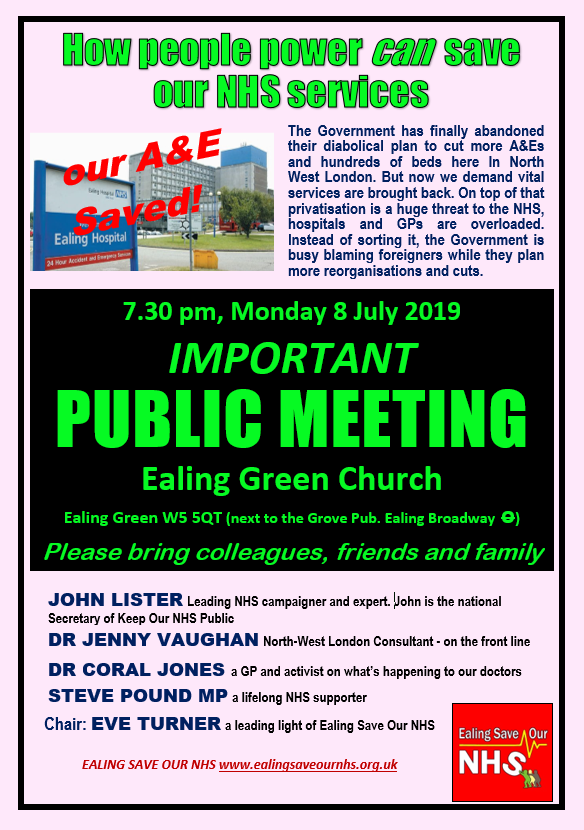
| This was planned before the announcement that the Shaping a Healthier Future plans were finally dead. So the focus of our meeting will be a bit different then our usual ‘Save Ealing Hospital’. We will certainly have a speaker on the Government’s NHS Long Term Plan and its impact on our local NHS, including GP services, and want to discuss where next for Ealing Hospital, now the axe has been lifted. – please watch this space for updates |
| Ealing Save Our NHS has had a lively and imaginative contingent on the Carnival Procession for the last few years and this year we plan to participate again. Unlike previous years we may be more in Carnival spirit as we have much to celebrate. No doubt our much photographed bed will still make an appearance. |