Our NHS in Crisis: ‘Transformation’ Special Issue
Issue 77
8 April 2019
‘Transformation’ Special Issue
The cancellation of the NHS North West London (NWL) ‘Shaping a Healthier Future’ (SaHF) plan on 26 March 2019 was an event of local, regional and national significance.
The central tenet of SaHF – the reduction in the number of Acute/Major hospitals – has been with us as a ‘transformation’ shibboleth for a number of years. A paper by American management consultant gurus McKinsey & Co published in 2009 famously alleged that 40% of all patients in Acute Hospital beds should not be there. (It’s hard to find any empirical evidence which supports what has become a ’Tablet of Stone’). McKinseys repeated this dogma at a World Economic Forum (WEF) meeting in Davos in April 2012. Attendees at that WEF meeting included the current Chief Executive, ex-Medical Director and the Strategy Director of NHS England (NHSE), two ex-Secretaries of State for Health, Liz Kendall MP, the bosses of BMI Health and the Nuffield Trust and the NHS property disposal expert, Robert Naylor.
A Failed Acute Reconfiguration Transformation
SaHF, announced in summer 2012, embodied the McKinsey metric and proposed closing 37% of the Acute hospital capacity in NWL in ‘at least three years’. On the ground that amounted to downgrading four of the nine Acute /’Major’ hospitals and transforming them into ‘Local’ hospitals with no A&E, no Intensive Care Unit, and no operating theatres. SaHF promised NWL’s 2.1 million residents ‘…changes that will improve care both in hospitals and the community…’. Also promised was ‘world -class healthcare outside of hospital’ in GP surgeries and in health centres. ‘Networks of GP practices will work with other providers of health and social care services to deliver co-ordinated healthcare to the local community.’ Cost savings of 4% would be achieved annually.
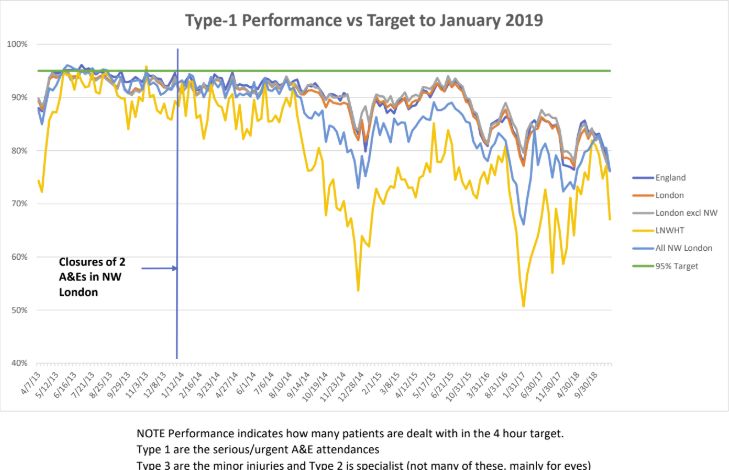
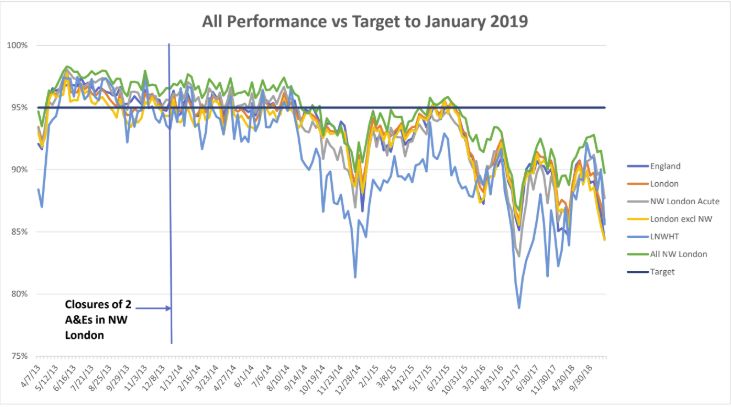
In September 2014 the SaHF closure of the A&E units at two NHS NWL Acute/Major hospitals decimated A&E performance throughout NWL to quickly become the worst in England. The two further A&E unit closures planned were delayed/abandoned and to this day the regional A&E performance has still not recovered. However the SaHF threat of downgrading Charing Cross and Ealing District General Hospitals has hung over the staff at these hospitals like the Sword of Damocles for almost seven years. Yet more grief was to be visited on Ealing Hospital in 2015 when Maternity was closed and in 2016 when Paediatrics was closed.
Inadequate SaHF Business Case
NHS NWL SaHF bosses ploughed ahead and in 2016 revealed more details of their business case. The SaHF ImBC Strategic Outline Case (SOC) for Acute reconfiguration 1 and 2 emerged. SOC1 covered building works required in ‘outer’ NWL hospitals, GP surgeries, and new Primary Care/out of hospital Hubs. £513 million was the breathtaking capital request. SOC2 covered building work in ‘inner‘ NWL and was estimated at £314 million. SOC1 was refused by NHS Improvement (NHSI) and NHSE London in September 2017. A second attempt at SOC1 occurred in July 2018 with a more modest capital request of £260 million. This was refused by implication in 2018 and finally went down in flames on 26 March 2019. The SOC2 capital request was never formalised and it was quietly buried by SaHF bosses in 2018.
Apart from Austerity and Brexit, what really killed the SaHF was its Acute reconfiguration business case proposition that Non Elective Admissions (NELs) – largely Emergency admissions – could be reduced significantly over time (probably by the McKinsey magical 40%). SaHF completely failed to convince NHSI and NHSE London financial bosses that it was making any progress at all to meet its own imposed annual NELs reduction target of 99,000 by 2025/26. Since 2013 no amount of increased GP or community services, specific new treatments or attempts to make more efficient use of hospital beds has had any impact on the annual level of NELs in NWL. In fact the total annual of NELs in 2017/18 were 181,632 and in 2013/14 they were 167,222. ‘Bed blocking’ didn’t help either. Elderly patients can’t be discharged if no places are available in care/nursing homes or family support is not available at home. Another major category is mentally ill patients. If no specialist mental health bed can be found then a patient can’t be discharged from an Acute hospital.
What Did SaHF Actually Cost?
Researcher Colin Standfield calculated in November 2017 that the management consultancy spend by NHS NWL since 2009/10 amounted to over £88 million. He recently re-calculated this and got it down to ‘just’ £72 million. Much, if not all, of this was SaHF related. There’s no easy way of calculating what the staff salary bill might have been for SaHF as it was a project and not a statutory NHS body.
Who Can be Held Responsible for the SaHF Failure?
Of the eight NHS NWL Clinical Commission Group (CCG) Chairs who signed their names to SaHF in 2012, four of them are still in post. They are Dr Mohini Parmar, Dr Tim Spicer, Dr Ian Goodman and Dr Nicola Burbidge. At least two of them are earning over £100,000/year. They must all consider their positions. The original SaHF Medical Director, Dr Mark Spencer moved into management consultancy a few years ago. However the current SaHF Medical Director, Susan La Brooy should also consider her position. The two NHS NWL Chief Officers behind the failed SaHF SOC1 £513 million bid (Clare Parker and Rob Larkman) gracefully resigned their posts in 2018. However the Accountable Officer responsible for the 2018 failed SaHF SOC1 £260 million bid, Mark Easton, is still in post and he surely must consider his position. Juliet Brown, Director of SaHF Implementation, must surely be made redundant.
What Can the Failed SaHF Tell us About Current and Future Transformations Like STPs and ICSs?
I find it hard to believe that all 44 NHS areas/’footprints’ were allowed to spend tens of £millions on management consultants to design’ prototype’ Acute reconfiguration projects. The 44 October 2016 Sustainability & Transformation Plans (STPs) throughout England borrow hugely from the SaHF approach (albeit with the addition of integrated healthcare and social care, and mental health). With SaHF failing, this calls into question the whole STP approach. Since 2017, STPs have morphed into Sustainability & Transformation Partnerships (again confusingly called STPs). In NWLthe STP was renamed the North West London Health and Care Partnership (HCP). The new NHS Long Term Plan has determined that all STPs will become Integrated Care Systems (ICSs) by April 2021.
NHS NWL STP Transformation To Be ‘Retired’?
Probably the primary goal of the NHS NWL STP/HCP is to plug the expected ‘do nothing’ annual funding gap of £1.41 billion by 2020/21. With just two years to go to meet this financial target who knows whether NHS NWL is on track to achieve this. Many commentators over the last two years have deduced that this financial STP target is unachievable and common sense tells me that they are right. I’m sure NHS NWL was disappointed to receive just £10 million funding in the 2018 round of national STP funding. There are plenty of SaHF ‘ghosts’ in the NHS NWL STP. One of them can be found in Delivery Area 5C. The downgrading of Ealing District General Hospital is cited here in the context of ‘…reducing demand for Acute services through investment in the proactive out of hospital care model enabled by investment in the Hubs’. We are back to Acute reconfiguration here and the need to radically reduce the number of NELs, which NHS NWL has failed miserably to do for over five years. Requests for capital funding to build Hubs were turned down in 2017 and in 2018.
It’s abundantly clear from recent comments in public by Mark Easton that the NHS Long Term Plan (LTP) presents NHS NWL with an opportunity to abandon its failing STP/HCP and carry out ‘re-modelling’ to produce an NHS NWL Integrated Care System (ICS). The fatal flaw in this, I suspect, is there is no compelling evidence that integrating healthcare and social care services will result in better care outcomes and reduced overall costs.
Will the NHS NWL ICS Transformation Go ‘Full Term’
However, what is clearly needed now is a STP/HCP rewrite to produce a deliverable ICS plan, aligned with the LTP. The architects of this new plan should not be authors of the SaHF or the STP/HCP or their management consultants. What is needed is new blood to create a viable plan based upon clear assumptions and credible evidence.
It would be painfully sad if this newsletter had to report in 2021 that the NHS NWL ICS was to be ‘re-modelled’ and replaced by a new acronym/plan. Surely at some point these repeated cycles of plan creation, failure, and re-branding have to come to an end and be replaced by stable, sustainable, adequately funded and maintained care services.
Finally what could tell us all a lot more about how and why SaHF failed is an independent Government inquiry or even an independent project review carried out by informed individuals who have had no involvement with SaHF. Surely by this means some valuable lessons could be learned from this expensive and, for some, painful failed attempt at transformation?
Eric Leach